Executive Summary
- Medetomidine, a veterinary sedative, is rapidly replacing xylazine as an adulterant in the illicit drug supply, particularly in Philadelphia, Chicago, and Pittsburgh.
- Withdrawal from medetomidine causes severe autonomic dysfunction, including hypertension and tachycardia, often requiring intensive care unit (ICU) treatment and is resistant to standard opioid withdrawal medications.
- Dexmedetomidine, a related drug, has been found effective in treating medetomidine withdrawal, but its use necessitates ICU-level care, straining healthcare resources.
Event Overview
Medetomidine, an animal sedative, has emerged as a significant adulterant in the illegal drug supply, particularly in combination with fentanyl. This trend, first detected in North America in 2022, is causing severe health complications, including unusual and intense withdrawal symptoms characterized by profound autonomic dysfunction. Reports from multiple cities, including Philadelphia, Pittsburgh, and Chicago, indicate a rapid increase in medetomidine-involved overdoses and hospitalizations, posing new challenges for healthcare providers and public health agencies already grappling with the opioid crisis. This shift complicates overdose reversals and requires specialized treatment protocols, often involving intensive care.
Media Coverage Comparison
| Source | Key Angle / Focus | Unique Details Mentioned | Tone |
|---|---|---|---|
| Centers for Disease Control and Prevention (MMWR) | Characterizing medetomidine withdrawal syndrome and increasing awareness among healthcare providers. | Presents data from three Philadelphia health systems showing 165 patients hospitalized with severe withdrawal symptoms, 91% requiring ICU care, and 83% responding to dexmedetomidine. All 55 patients tested at one health system were positive for 3-hydroxy medetomidine. | Informative and clinical, emphasizing public health implications. |
| The Philadelphia Inquirer | The alarming rise of medetomidine in Philadelphia's drug supply and its impact on emergency rooms. | Highlights the rapid replacement of xylazine by medetomidine, with 72% of illicit opioids testing positive for medetomidine in late 2024. It mentions paramedics finding overdose victims unresponsive to naloxone and the need for ICU treatment due to severe withdrawal symptoms. | Concerned and urgent, emphasizing the challenges faced by medical professionals. |
| STAT News | Medetomidine replacing xylazine and causing excruciating withdrawal symptoms. | Emphasizes that medetomidine is replacing xylazine due to crackdowns, resulting in severe health complications and potentially deadly withdrawal. Quotes Dr. Sam Huo on the challenges of predicting severe withdrawal and the impact on opioid withdrawal management. | Analytical and concerned, focusing on the medical and policy implications of the shift. |
Key Details & Data Points
- What: Medetomidine, a veterinary sedative, is increasingly being used as an adulterant in illicit drugs, primarily fentanyl, leading to severe withdrawal symptoms and complicating overdose treatments.
- Who: People who use drugs (PWUD) are the primary affected population. Healthcare providers, public health agencies, and researchers are actively involved in identifying, treating, and studying the effects of medetomidine.
- When: The rise of medetomidine has been observed since 2022, with significant increases in cases reported from mid-2024 to early 2025. Philadelphia saw a rapid increase in medetomidine detection from May to November 2024.
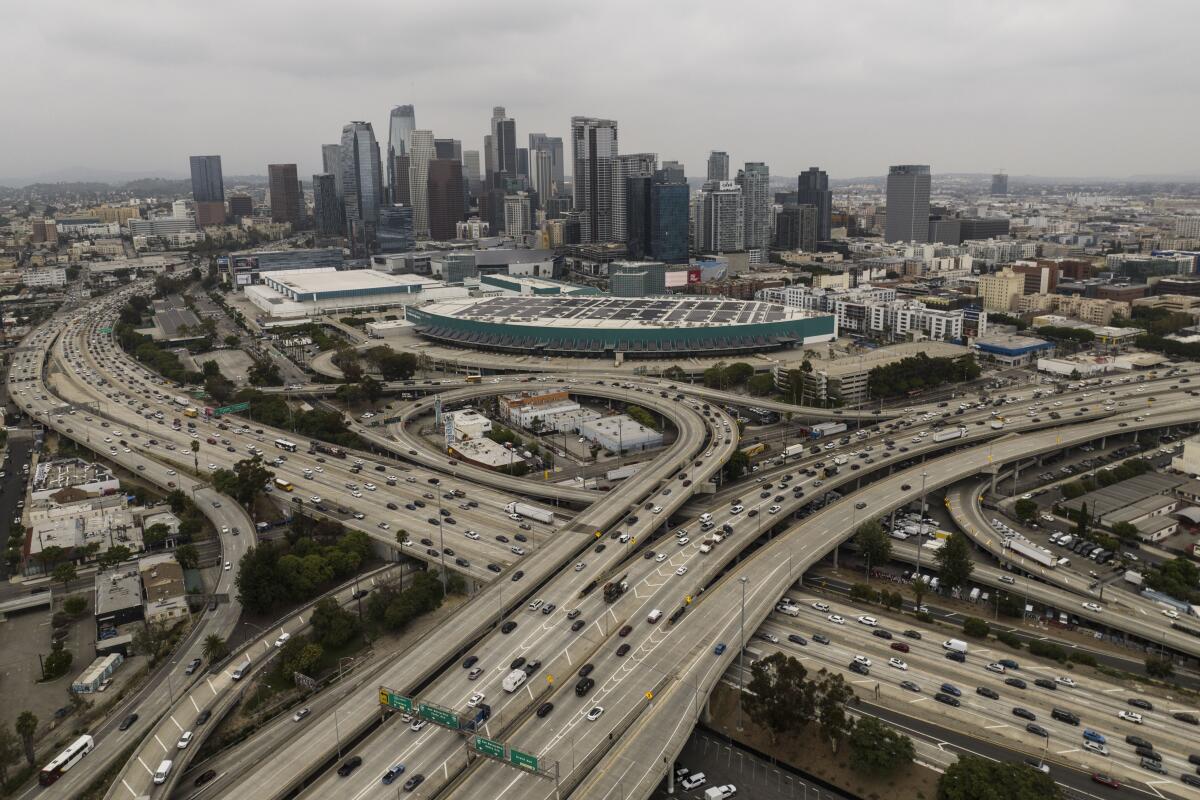
- Where: The issue is prominent in cities like Philadelphia, Pittsburgh, and Chicago, but the problem is becoming more widespread in the US.
Key Statistics:
- Key statistic 1: 72% (of illicit opioid samples tested in Philadelphia in late 2024 contained medetomidine)
- Key statistic 2: 91% (of patients hospitalized for medetomidine withdrawal in Philadelphia required ICU care)
- Key statistic 3: 83% (of patients treated with dexmedetomidine experienced a decrease in withdrawal symptoms)
Analysis & Context
The emergence of medetomidine as a drug adulterant represents a significant challenge to public health efforts to combat the opioid crisis. Its rapid rise, particularly as a replacement for xylazine, indicates a dynamic shift in the illicit drug market in response to law enforcement efforts. The severe withdrawal symptoms associated with medetomidine place a substantial burden on healthcare systems, requiring specialized treatment and ICU-level care. The fact that standard opioid overdose reversal medications are less effective in cases involving medetomidine further complicates the situation. Further research is needed to understand the long-term health effects of medetomidine use and to develop more effective strategies for prevention and treatment.
Notable Quotes
The supply has just shifted so heavily from xylazine to medetomidine, and there is an overwhelming amount of medetomidine in the supply. With withdrawal from medetomidine, severe cases can be life-threatening. And the scary part is that we don’t have a way right now to predict who will be at risk for severe withdrawal and who’s not.
Conclusion
The rapid surge of medetomidine in the illicit drug supply represents a critical public health crisis that demands urgent and multifaceted responses. Its presence, frequently in combination with fentanyl and xylazine, is associated with severe withdrawal symptoms, including hypertension, tachycardia, agitation, intractable vomiting, excessive diaphoresis, and a waxing and waning hypoactive encephalopathy, placing a significant strain on healthcare resources, particularly ICUs. The increasing prevalence of medetomidine, which has now surpassed xylazine in some regions, complicates overdose response, as its sedative effects are not reversed by naloxone, potentially leading to prolonged sedation, bradycardia, and hypotension. Dexmedetomidine has shown effectiveness in managing medetomidine withdrawal, but its administration often necessitates intensive medical intervention. Enhanced monitoring of drug supply trends through community-level drug checking programs, expanded toxicological testing, and real-time data sharing among healthcare providers and public health agencies are crucial for effectively addressing this emerging threat. Furthermore, the development and distribution of medetomidine test strips, similar to those available for fentanyl and xylazine, could empower individuals to make more informed decisions about their drug use and reduce harm. A comprehensive harm reduction strategy should include wider accessibility of naloxone, overdose prevention education, and evidence-based wound care practices, given medetomidine's potential association with vasoconstriction and related tissue damage.
Disclaimer: This article was generated by an AI system that synthesizes information from multiple news sources. While efforts are made to ensure accuracy and objectivity, reporting nuances, potential biases, or errors from original sources may be reflected. The information presented here is for informational purposes and should be verified with primary sources, especially for critical decisions.